Emma Hansen, Quinn Kahle, Aris Magoulas, Ryan Lundeen
Overview
The medical field currently lacks sufficient technology to properly train residents and fellows learning interventional lumbar spine procedures; many trainees begin by performing procedures on actual patients without prior practice in a simulated environment. This lumbar spine procedure model aims to alleviate risks for patients and allow trainees to build confidence before executing procedures on actual people. This model aims to provide a three-dimensional anatomical representation that enables trainees to gain experience executing interventional spine procedures on various vertebral pathologies. This is a former BME design project in collaboration with UW Health that is currently in its 6th semester.
Lumbar spine injections are a fairly common, low-risk procedure used as a pain management technique. The current standard for teaching lumbar spine procedures involves having residents and fellows immediately perform procedures on patients without hands-on practice in a simulated environment [1]. Simulation devices have recently become a viable alternative to train individuals, allowing them to build skills for more complex injections. Simulation devices allow new physicians to become comfortable with the procedure without the risk of learning on patients. These devices typically replicate the lumbar region of the body. Many contain a replica spine, replica cerebrospinal fluid, and replica tissue, as well as circuitry to power various components of the device. However, these devices are expensive, ranging in cost from $1000-$5000 [2, 3]. Additionally, most current models fail to replicate alternative spinal pathologies, such as scoliosis, which limit their function as an educational tool. Significant improvements can be made to lumbar injection models to reduce their cost and increase the simulated variability in the educational procedure. In previous semesters, multiple prototypes have been produced including that of a “normal” lumbar region as well as a scoliotic model.
Currently, our team is working to use SLA printing rather than FFF, which has been used in previous semesters. By doing this, we aim to reduce cost and make the model more reproducible while maintaining properties of cortical bone under fluoroscopic imaging.
Material Selection/SLA Justification
Some polymers that have been used with vat polymerization for bone tissue engineering applications include poly(propylene fumarate) (PPF) and poly(?-caprolactone fumarate) (PCLF) as well as PPF/PCLF blends. Supplementing these polymers with hydroxyapatite (HA) nanoparticles has been shown to increase the elastic modulus and properly mimic bone structure and density. The advantages of SLA that are applicable for our project goals include, (1) the fine resolution enables layer thicknesses as small as 100 ?m, (2) the tunability of the scaffold stiffness due to the variety of polymers that can be printed and the degree to which crosslinking can be controlled. Unfortunately SLA is constrained to photo-curable polymers and can be limited in terms of the amounts of ceramic additives. As a result of this we have chosen to use HA powder with resin.
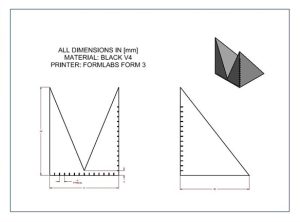
One drawback of the previous design printed using FFF was the need for a special, barium doped filament to have a realistic appearance under fluoroscopy. Not only was this filament expensive, but due to supply chain issues it was difficult to source since it was manufactured in Brazil. One way we hope to improve on the original design is to reduce the material constraint by utilizing domestically available, less expensive powders and mixing them into uncured resin for use in SLA manufacturing. We designed and printed a test part using FormLabs Black V4 to determine baseline Hounsfield Unit measurement of the material. We will then use these measurements, as well as ones from true lumbar spines and the FFF parts to choose the best material and additive combination.
Printing a Test Part
A test part was printed via SLA (FormLabs Form 3, Black V4) at the MakerSpace. The test part was designed to test both solid Black V4 of varying thickness, as well as the effect of an air gap in the part to determine if a hollow vertebra design is feasible. The hollow design would decrease material usage and print time, but the air gap may reduce the Hounsfield too far and make the design not realistic enough. Our goal is to create one model of the Hounsfield reading as a function of thickness and another model of the Hounsfield reading as a function of thickness with an air gap. We will then design and print test samples with varying amounts of powder additives, use fluoroscopy to measure their Hounsfield Units and apply them to the model determined from the test part. By getting fluoroscopic images of the part with the same imaging technology used in real lumbar spine procedures, we can determine which infill settings will produce the most realistic lumbar vertebrae. The team originally planned to go to the Madison Surgery Center prior to this week to view the part under fluoroscopy; however, this was not possible due to our client’s busy schedule. We will go obtain images within the next couple days when our client is available.

3D Rendering of Lumbar Spine Model
We anticipate most of our end users to not be familiar with 3D printing or polymer processing in general. One goal for this project is to provide potential end users with the tools to print the design and use it with as little pre and post processing as possible. To provide our end users with a simple, plug-and-play design, we have created pre-sliced .stl files that can be downloaded and printed without the need for the user to manipulate or optimize the printing process in any way.

These models not only provide consistent and accurate placement of the vertebrae, but also a simple and efficient way to secure the vertebrae in the gel matrix, reducing the complexity of the overall design.
After we get a set of baseline measurements, we will reassess the design of the vertebrae to best match the Hounsfield Unit measurement of human bone. Since the fluoroscope is only used to observe the spine from one direction, we could take advantage of non-uniform scaling in the FormLabs slicing software to increase the amount of material in the direction of the fluoroscope reading to better improve the realism of the specimen.
Printing Plan
Some key steps we plan to follow while SLA printing vertebrae are as follows:
- Use new composite powders to mix with original resin for SLA prints. Hydroxyapatite, calcium carbonate, and calcium phosphate are all options that could get the properties of our replica vertebrae closer to that of actual bone [4].
- Keep adding powder in specified increments so it is not necessary to use multiple batches of resin. For example – create a 0.5% powder/resin batch, then add the same increment to the next batch to achieve 0.1%
Next Steps
Within the next couple days, the team plans to go to the Madison Surgery Center to obtain fluoroscopic images of the test part. At this time, we will also be able to pick up the hydroxyapatite powder that was ordered. We can then print parts using the HA and calcium carbonate doped resins and get fluoroscopic images of these parts to compare with cortical bone. Based on our timeline with the end of the semester approaching, we will see if additional modifications can feasibly be made.
References
[1] V. Manoharan, D. van Gerwen, J. J. van den Dobbelsteen, and J. Dankelman, “Design and? validation of an epidural needle insertion simulator with haptic feedback for training resident anaesthesiologists,” in 2012 IEEE Haptics Symposium (HAPTICS), Mar. 2012, pp. 341–348, doi: 10.1109/HAPTIC.2012.6183812.
[2] “Spinal Injection Simulator,” GTSimulators.com.? https://www.gtsimulators.com/products/spinal-injection-simulator-lf01036u (accessed Dec. 09, 2020).
[3] “Imaging Course Trainer – Lumbar Spinal Intervention Simulator for Image Guided Injections – 3B? Scientific.” https://www.a3bs.com/image-guided-lumbar-spinal-injection-trainer-p65-1021898-p65-3b-scientific,p_34_30509.html (accessed Dec. 09, 2020).
[4] Trombetta, R., Inzana, J. A., Schwarz, E. M., Kates, S. L., & Awad, H. A. (2016). “3D printing of calcium phosphate ceramics for bone tissue engineering and drug delivery”. Annals of Biomedical Engineering, 45(1), 23–44. https://doi.org/10.1007/s10439-016-1678-3