Emma Hansen, Quinn Kahle, Aris Magoulas, Ryan Lundeen
Project Background
The medical field currently lacks sufficient technology to properly train residents and fellows learning interventional lumbar spine procedures; many trainees begin by performing procedures on actual patients without prior practice in a simulated environment. This lumbar spine procedure model aims to alleviate risks for patients and allow trainees to build confidence before executing procedures on actual people. The function of the model is to provide a three-dimensional anatomical representation that enables trainees to gain experience executing interventional spine procedures on various vertebral pathologies. This is a former BME design project in collaboration with UW Health that is currently in its 6th semester.
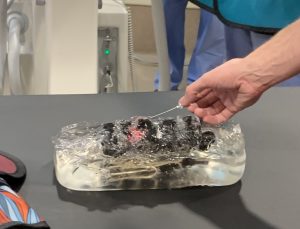
Lumbar spine injections are a fairly common, low-risk procedure used as a pain management technique. The current standard for teaching lumbar spine procedures involves having residents and fellows immediately perform procedures on patients without hand-on practice in a simulated environment [1]. Simulation devices have recently become a viable alternative to train individuals, allowing them to build skills for more complex injections. Simulation devices allow new physicians to become comfortable with the procedure without the risk of learning on patients. These devices typically replicate the lumbar region of the body. Many contain a replica spine, replica cerebrospinal fluid, and replica tissue, as well as circuitry to power various components of the device. However, these devices are expensive, ranging in cost from 1000 to 5000 dollars [2, 3]. Additionally, most current models fail to replicate alternative spinal pathologies, such as scoliosis, which limit their function as an educational tool. Significant improvements can be made to lumbar injection models to reduce their cost and increase the simulated variability in the educational procedure.? In previous semesters, multiple prototypes have been produced including that of a “normal” lumbar region as well as a scoliotic model.
Preliminary Design and Manufacturing Considerations
In existing prototypes, lumbar vertebrae L1-L5 are 3D printed using XCT-B filament via FFF. XCT-B filament consists of Acrylonitrile Butadiene Styrene (ABS) filament doped with barium sulfate (BaSO4) [4]. This filament has worked well for printing vertebrae because it has a has a known radiopacity of -200 Hounsfield Units (HU) at 100% infill, while L1-L4 have a similar radiopacity of 132.6 ± 42.9 HU [5]. Hounsfield Units measure relative radiodensity in CT imaging [5]. The goal is to have the 3D printed vertebrae look as similar to actual bone as possible on fluoroscopy.
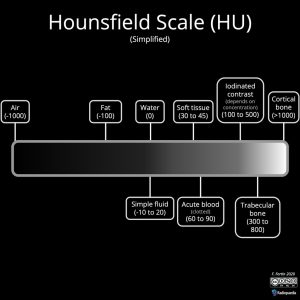
While XCT-B produced fairly realistic images, this filament is relatively expensive and difficult to acquire. With the end goal of creating an affordable and accessible model, improvements could be made in this area. Multiple prints will be necessary to create each of the five lumbar vertebrae.
Additionally, current devices on the market do not include satisfactory needle placement feedback. This is vital so that the individual performing the injection is aware if they are performing it correctly. Previous strategies implemented to incorporate needle feedback include a circuit using an Arduino microcontroller, a liquid sensor, and conductive paint. Of these three, the Arduino circuit was the most effective. However, the needle feedback aspect should be refined prior to use by medical professionals.
Furthermore, all materials used should be compatible with an X-Ray machine and durable as well as safe for consistent human touch, compatible with medical needles and possible indicator fluids that users may inject to simulate procedures, and must maintain standards of shelf life and life in service.
Goals
This semester, our team plans to improve upon the current prototypes of the lumbar spine procedure model using 3D printing and other technologies to provide medical staff with a more effective training experience. We will accomplish this by implementing the following:
- Use SLA rather than FFF to produce vertebrae. This could increase the realism of the model and decrease manufacturing cost.
- Dope SLA resin with an additive. If possible, this strategy could get us closer to the appropriate Hounsfield units for vertebral bone.
- Test different thicknesses of SLA epoxy to determine if an additive is necessary.
- Create an interactive SolidWorks model allowing users to accommodate different spinal pathologies.
- Integrate user feedback via packets in the “epidural space” filled with colorized titration solutions.
Next Steps
Our team will be meeting with our client (physician at UW Health) in the near future to discuss semester plans and get feedback on our new design ideas. We will then begin fabrication using SLA and start developing a SolidWorks model. Additionally, we plan to test our improved device at the Madison Surgery Center prior to the end of the semester, where we will receive additional feedback from medical professionals.
References
[1] V. Manoharan, D. van Gerwen, J. J. van den Dobbelsteen, and J. Dankelman, “Design and? validation of an epidural needle insertion simulator with haptic feedback for training resident anaesthesiologists,” in 2012 IEEE Haptics Symposium (HAPTICS), Mar. 2012, pp. 341–348, doi: 10.1109/HAPTIC.2012.6183812.
[2] “Spinal Injection Simulator,” GTSimulators.com.? https://www.gtsimulators.com/products/spinal-injection-simulator-lf01036u (accessed Dec. 09, 2020).
[3] “Imaging Course Trainer – Lumbar Spinal Intervention Simulator for Image Guided Injections – 3B? Scientific.” https://www.a3bs.com/image-guided-lumbar-spinal-injection-trainer-p65-1021898-p65-3b-scientific,p_34_30509.html (accessed Dec. 09, 2020).
[4] “Filamentos para Impressoras 3D.” http://www.3don.net.br/Informacoes.aspx?abschnitt=XCT#XCT (accessed Apr. 27, 2021).
[5] Savi, M. A. B. Andrade, and M. P. A. Potiens, “Commercial filament testing for use in 3D printed phantoms,” Radiation Physics and Chemistry, vol. 174, p. 108906, Sep. 2020, doi: 10.1016/j.radphyschem.2020.108906.